The journey of pituitary tumor surgery represents a complex intersection of neuroendocrinology, neurosurgical innovation, and postoperative care. Historically, surgical intervention for pituitary masses dates back to the early 20th century, with the advent of transsphenoidal approaches marking a pivotal shift towards minimally invasive procedures. Over the decades, advances in imaging, surgical techniques, and endocrinological management have significantly transformed patient outcomes. Yet, despite these progresses, postoperative challenges persist that require careful navigation. This article explores the origins, evolution, and contemporary strategies in overcoming common challenges in pituitary tumor recovery, emphasizing evidence-based practices cultivated through decades of clinical experience and research.
The Evolution of Pituitary Tumor Surgery: From Early Techniques to Modern Approaches
Understanding current postoperative challenges necessitates a historical perspective. Initially, pituitary tumors were diagnosed via crude imaging and treated with craniotomies—an invasive approach fraught with high morbidity. The pioneering work of Dr. Harvey Cushing in the early 1900s laid foundational principles for neurosurgical intervention, emphasizing meticulous technique and the management of hormonal disturbances. However, it wasn’t until the 1960s that the transsphenoidal approach gained prominence, initially through microscopic techniques, and later supplemented by endoscopic methods. This evolution paralleled advancements in neuroimaging, including computed tomography (CT) scans and magnetic resonance imaging (MRI), allowing for precise tumor localization and surgical planning.
Current Surgical Paradigms and Their Impact on Recovery

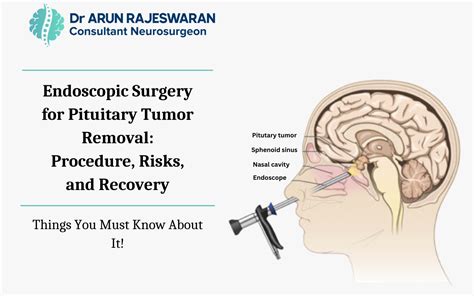
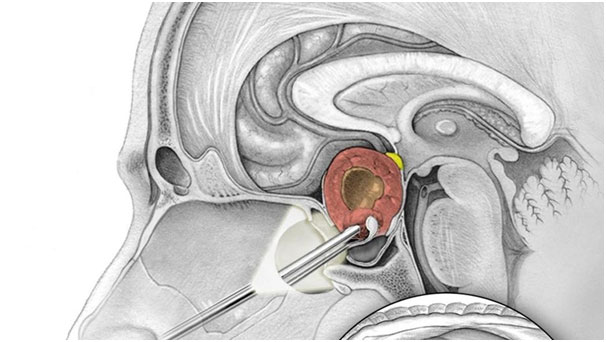
Today, the transsphenoidal route—particularly endoscopic transnasal approaches—has become the gold standard for most pituitary adenomas. Its advantages include reduced cranial trauma, decreased hospital stay, and quicker recovery times. Nevertheless, postoperative challenges remain, including hormonal dysregulation, cerebrospinal fluid leaks, neurological deficits, and infection risks. Addressing these requires a multidisciplinary strategy integrating neurosurgery, endocrinology, speech therapy, and rehabilitation services, all tailored to individual patient profiles.
Addressing Hormonal Imbalances Post-Surgery
One of the earliest and most persistent challenges following pituitary surgery involves hormonal disturbances. The pituitary’s central role in endocrine regulation means that even minimal intraoperative manipulation can disrupt hormone secretion patterns. Patients may experience transient or permanent deficiencies in hormones such as ACTH, TSH, GH, LH, and FSH. Historically, cortisol replacement therapy was initiated empirically, often leading to complications of over- or under-replacement. Advances in intraoperative cortisol monitoring, coupled with refined endocrinological assessment protocols, now enable more precise hormone management, reducing long-term deficits.
| Relevant Category | Substantive Data |
|---|---|
| Postoperative Hypopituitarism Incidence | Approximately 25-50% in various series, depending on tumor size and invasiveness |

Preventing and Managing Cerebrospinal Fluid Leaks
Cerebrospinal fluid (CSF) leaks rank among significant postoperative complications, historically associated with morbidity such as meningitis or pneumocephalus. The advent of the nasoseptal flap technique, first described in the early 2000s, revolutionized the prevention of postoperative leaks. By providing a vascularized tissue barrier, this method ensures durable closure of the sellar floor, reducing leak rates to below 5%. Early identification of leaks and prompt surgical repair—often with autologous tissue—are critical to prevent sequelae. Continuous refinement of closure techniques demonstrates an ongoing commitment to minimizing this challenge.
Neurological and Visual Outcome Optimization
Postoperative neurological deficits, especially visual impairment, are pressing concerns given the proximity of the tumor to the optic apparatus. Historically, intraoperative neuronavigation and intraoperative MRI guidance have significantly reduced iatrogenic injury. Effective decompression of sellar and parasellar structures often results in improved or preserved visual function. However, surgical trauma or edema can impair recovery. Early intervention with corticosteroids to reduce cerebral edema and structured visual rehabilitation enhance recovery trajectories, demonstrating the importance of multidisciplinary postoperative care.
| Relevant Category | Substantive Data |
|---|---|
| Visual Improvement Rate | Approximately 70-80% of patients experience significant visual improvement post decompression |
Key Points
- Accurate preoperative imaging combined with intraoperative navigation minimizes complications.
- Monitoring and managing hormonal disturbances via individualized hormone replacement are essential for restoring function.
- Effective closure techniques, such as vascularized nasoseptal flaps, substantially reduce CSF leak risks.
- Early detection and intervention optimize neurological and visual recovery outcomes.
- Multidisciplinary collaboration remains central to overcoming postoperative hurdles in pituitary tumor surgery.
Modern Strategies and Innovations in Managing Postoperative Challenges
Technological integration continues to advance postoperative care paradigms. Real-time intraoperative MRI provides immediate feedback, easing the complexity of tumor resection and minimizing residual tissue. Meanwhile, minimally invasive nasal endoscopy reduces tissue trauma and expedites recovery. The emergence of refined biomarkers and dynamic testing enhances early detection of hormonal deficits, enabling preemptive interventions. Furthermore, patient-centered rehabilitation programs, including physical therapy and psychological support, address the broader impact of surgery on quality of life.
Personalized Medicine and Predictive Analytics
Emerging evidence supports the role of predictive models based on preoperative tumor characteristics and genetic profiles. These models assist in anticipating postoperative complications, allowing for customized perioperative care plans. As data accumulates from multicenter registries, machine learning algorithms are increasingly capable of stratifying risk, thus optimizing resource allocation and improving outcomes. Yet, integrating such innovations into routine practice requires validation through prospective studies and standardized protocols.
| Relevant Category | Substantive Data |
|---|---|
| Predictive Model Accuracy | Initial studies report 80-85% accuracy in risk stratification for hormonal and complications |
Conclusion: Navigating the Recovery Landscape with Evidence-Based Precision
From the early days of invasive craniotomies to the sophisticated endoscopic techniques prevalent today, the surgical management of pituitary tumors has undergone transformative evolution. Despite this progress, challenges such as hormonal imbalances, CSF leaks, and neurological deficits continue to challenge clinicians. Integrating a nuanced understanding of historical approaches, technological innovations, and personalized care models paves the way for more favorable recovery trajectories. Future directions, driven by predictive analytics and regenerative medicine, promise further refinement in overcoming postoperative hurdles, ultimately elevating patient outcomes and quality of life.
What are the most common postoperative complications after pituitary tumor surgery?
+Common postoperative complications include hormonal deficiencies, cerebrospinal fluid leaks, visual disturbances, and neurological deficits. Advances in surgical methods and perioperative care are reducing these risks, but they remain significant considerations in patient management.
How can hormonal imbalances be effectively managed after surgery?
+Early detection through dynamic hormonal testing, coupled with personalized hormone replacement therapy, can restore endocrine function. Continuous monitoring and adjustment are vital for optimal recovery and long-term health.
What innovations have most improved postoperative outcomes in pituitary surgery?
+Technologies such as intraoperative MRI, vascularized nasoseptal flaps, and predictive analytics have significantly reduced complication rates and enhanced recovery, setting new standards in surgical care.