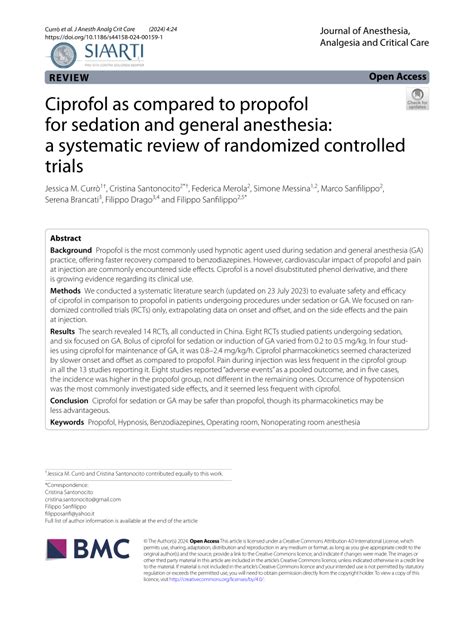
Deciding between sedation and general anesthesia for medical procedures is often a complex undertaking that blends clinical guidelines, patient preferences, and procedural intricacies. To the untrained eye, both modalities seem to aim at comfort and pain management, yet they operate at different depths of consciousness and involve distinct mechanisms, risks, and recovery trajectories. This layered decision-making process is not simply a matter of choosing what feels better but requires a nuanced understanding of the physiological, psychological, and logistical factors that can influence patient outcomes. Through an in-depth examination of sedation and general anesthesia, we can illuminate the critical factors influencing optimal choice and explore emerging considerations that may redefine standards of care.
Understanding Sedation and General Anesthesia: Core Principles and Distinctions

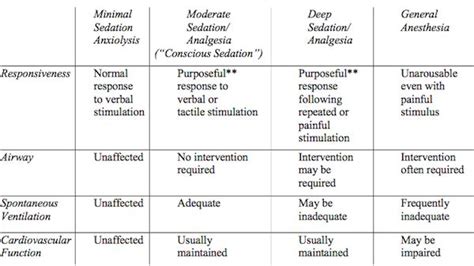
Sedation typically refers to a spectrum of drug-induced states that reduce anxiety and discomfort without rendering the patient unconscious. It spans from minimal sedation, where patients remain responsive, to deep sedation, where responses may be limited, but not to the extent of loss of protective reflexes. The primary agents involved include benzodiazepines, opioids, and sometimes propofol at lower doses, all administered under strict monitoring protocols. Its utility extends across various outpatient procedures such as dental surgeries, endoscopies, and minor orthopedic interventions.
General anesthesia, by contrast, induces a reversible state of unconsciousness, analgesia, amnesia, and muscle relaxation, achieved through a combination of intravenous drugs and inhalational agents. It involves a more profound suppression of central nervous system activity, necessitating airway management through intubation or supraglottic devices, alongside continuous monitoring of vital signs, gas concentrations, and neurological status. The broad applicability of general anesthesia ranges from complex surgeries like cardiac repairs to elaborate neurosurgical procedures where optimal control over physiological variables is critical.
Technological Advances and Precision in Anesthetic Delivery

Recent innovations in anesthesia technology have transformed the landscape of sedation and general anesthesia. Target-controlled infusion (TCI) systems and closed-loop feedback mechanisms allow anesthesiologists to tailor drug delivery dynamically, ensuring stability and minimizing side effects. For sedation, patient-controlled analgesia (PCA) devices empower patients with autonomy over pain management, effectively reducing anxiety and discomfort during outpatient settings.
In the realm of general anesthesia, anesthesia information management systems (AIMS) provide real-time data analytics, enhance safety protocols, and streamline multi-modal monitoring. These advances underpin personalized anesthesia care plans, tailoring depth and duration to individual patient physiology and procedure specifics, ultimately improving safety profiles and recovery times.
| Relevant Category | Substantive Data |
|---|---|
| Monitoring Accuracy | Use of multi-parameter monitors (EEG, BIS) reduces intraoperative awareness risk to less than 0.1% |
| Drug Delivery Precision | Automated TCI systems can adjust propofol infusion rates with ±5% accuracy based on pharmacokinetic models |
| Recovery Times | Advances in drug formulations have decreased average emergence times for general anesthesia from 20–30 mins to approximately 10–15 mins in many cases |
When Is Sedation the Best Choice? Evaluating Indications and Limitations
Based on extensive clinical data, sedation is often preferable when procedures are minimally invasive, outpatient in nature, and involve low risk for complications. Procedural context dictates the depth of sedation, with minimal and moderate sedation adequately managing pain and anxiety for interventions such as colonoscopies, biopsies, and certain dermatological procedures.
However, sedation’s limitations become apparent when considering factors such as patient comorbidities—especially those involving airway or respiratory compromise—and cases that demand complete muscular relaxation or unconsciousness. The possibility of intra-procedural movement, inadequate analgesia at deeper levels, or patient agitation can compromise outcomes. Moreover, the reliance on patient cooperation and responsiveness makes sedation less suitable for uncooperative or pediatric populations. Even with technological adjuncts, sedation does not equate with the depth of unconsciousness achieved via general anesthesia, imposing constraints upon its application in certain high-risk scenarios.
Case studies: Effective applications of sedation
In a 2022 multicenter trial, sedation was successfully employed during outpatient transcatheter aortic valve implantations, resulting in 85% fewer adverse respiratory events compared to general anesthesia, primarily because patients maintained spontaneous ventilation. Similarly, advanced sedation protocols with opioid-sparing techniques have demonstrated efficacy in reducing postoperative nausea and hospital stay durations in bariatric procedures.
| Relevant Category | Data/Outcome |
|---|---|
| Success Rate | Over 95% success in minor outpatient procedures with sedation |
| Complication Rate | Lower incidence of respiratory complications (<1%) in sedation versus general anesthesia (2–3%) |
When Is General Anesthesia Necessary? Critical Considerations and Risks
In contrast, general anesthesia remains indispensable in surgeries requiring complete unconsciousness, such as complex cardiac surgeries, neurosurgeries, or when airway management and precision in physiological control are paramount. The depth of anesthesia allows for excellent surgical conditions, minimized patient movement, and advanced control of hemodynamic parameters.
Nonetheless, general anesthesia is not without risks. Potential adverse events include hypotension, postoperative nausea and vomiting, cognitive disturbances, and rare but serious complications like malignant hyperthermia. Anesthesia-related mortality rates are low but remain at approximately 1 in 100,000 cases in developed healthcare environments, emphasizing the importance of expert administration and vigilant monitoring.
Technological advances mitigating risks
Implementation of volatile anesthetic agents with favorable safety profiles, along with residual effect monitoring, has diminished the likelihood of intraoperative awareness and postoperative delirium. Additionally, protocols like Enhanced Recovery After Surgery (ERAS) recommend multimodal analgesia and early mobilization to reduce anesthesia-related morbidity.
| Relevant Category | Data/Outcome |
|---|---|
| Conversion Rate | Unplanned conversion from sedation to general anesthesia occurs in <1% of cases, mainly due to inadequate sedation or airway compromise |
| Complication Reduction | Use of BIS-guided anesthesia reduces hypotension incidence by 25% |
| Recovery Time | Standard general anesthesia involves ~10–15 mins for emergence with optimized protocols |
Patient-Centered Decision-Making: Balancing Risks, Benefits, and Preferences
Choosing between sedation and general anesthesia offers a unique opportunity to incorporate patient preferences into clinical decisions. Shared decision-making models advocate for transparent discussions about procedural risks, expected recovery trajectories, and individual health considerations. For example, patients with obstructive sleep apnea or significant cardiopulmonary comorbidities may prefer procedural sedation under enhanced monitoring to reduce anesthesia-related risk profiles.
Documentation of patient values, prior anesthesia experiences, and lifestyle factors further refines this process. In settings where patient autonomy and improved recovery outcomes are prioritized, the development of clear communication pathways ensures that nuanced preferences are appropriately integrated into clinical plans.
Informed consent as a dynamic process
Empowering patients with comprehensive, understandable information about sedation and general anesthesia fosters informed consent, mitigates procedural anxiety, and enhances satisfaction—an integral component of high-quality, patient-centered care. Digital tools, such as decision aids and virtual reality demonstrations, are increasingly employed to visualize procedural experiences, further supporting informed choices.
| Relevant Category | Data/Outcome |
|---|---|
| Patient Satisfaction | Studies indicate higher satisfaction scores when patients participate actively in anesthesia planning, with a 15% preference for sedation in outpatient procedures |
| Perceived Safety | Over 80% of patients correctly perceive sedation as lower risk than general anesthesia, influencing their choices despite clinical nuances |
Conclusion: Navigating the Balance — Which Is Right for You?
The decision matrix between sedation and general anesthesia hinges on a thorough assessment of procedural complexity, patient health status, risk tolerance, and personal preferences. While sedation offers a minimally invasive, lower-risk alternative suited for straightforward outpatient procedures, general anesthesia provides unparalleled control necessary for complex surgeries demanding complete unconsciousness and physiological stability.
Incorporating technological innovations, meticulous monitoring, and patient-centered communication enhances safety across both modalities. Practitioners skilled in tailoring anesthetic plans—respecting individual variability and procedural demands—are central to optimizing outcomes. Ultimately, the choice extends beyond clinical indications, embracing a nuanced appreciation of each patient’s unique context and values, ensuring care is as safe as it is aligned with personal comfort and preferences.
Key Points
- Understanding the depth and scope of sedation versus general anesthesia guides appropriate application based on procedure and patient health.
- Technological progress in monitoring and drug delivery enhances safety, enabling precise, personalized anesthetic care.
- Patient preferences, risk profiles, and procedural complexity remain foundational in choice, emphasizing the importance of shared decision-making.
- Emerging trends focus on minimally invasive, rapid recovery protocols that leverage advancements in pharmacology and digital communication.
- Expert anesthesia planning is critical in balancing safety, efficacy, and patient experience across diverse surgical and diagnostic contexts.
Can sedation be used for any surgical procedure?
+Not all procedures are suitable for sedation. The decision depends on the complexity, required depth of anesthesia, patient health, and potential airway risks. For major surgeries or those requiring complete immobilization and muscle relaxation, general anesthesia is typically necessary.
Is recovery faster with sedation or general anesthesia?
+Generally, sedation involves a quicker recovery, often allowing patients to return home the same day with minimal post-procedure effects. In contrast, general anesthesia usually requires a recovery period of 1-2 hours due to the depth of sedation and physiological effects.
What are the main risks associated with general anesthesia?
+Risks include cardiovascular instability, respiratory complications, postoperative nausea and vomiting, cognitive disturbances, and, rarely, allergic reactions or malignant hyperthermia. Proper monitoring and experienced anesthesia providers mitigate these risks significantly.
How do technological advances improve anesthesia safety?
+Innovations such as BIS monitoring, automated drug infusion systems, and real-time data analytics enable precise control over anesthesia depth, minimize human error, and reduce adverse events, leading to safer patient outcomes.
Can patient preferences influence the choice of anesthesia?
+Absolutely. Shared decision-making, informed by comprehensive discussions about risks, benefits, and personal comfort, ensures that the selected anesthesia modality aligns with patient values and expectations, ultimately improving satisfaction and adherence.