The evolution of minimally invasive therapies in urology has considerably expanded the therapeutic arsenal against benign prostatic hyperplasia (BPH). Among these, Prostatic Artery Embolization (PAE) has emerged as a promising alternative to traditional surgical interventions, gaining interest due to its less invasive nature and promising outcomes. However, as with any interventional procedure, understanding the array of potential risks is paramount for clinicians and patients alike. This article explores the common risks associated with PAE, delving into their mechanisms, incidence rates, and implications, prompting us to question: how can we optimize patient selection and procedural techniques to mitigate these risks?
Understanding Prostatic Artery Embolization: A Modern Technique

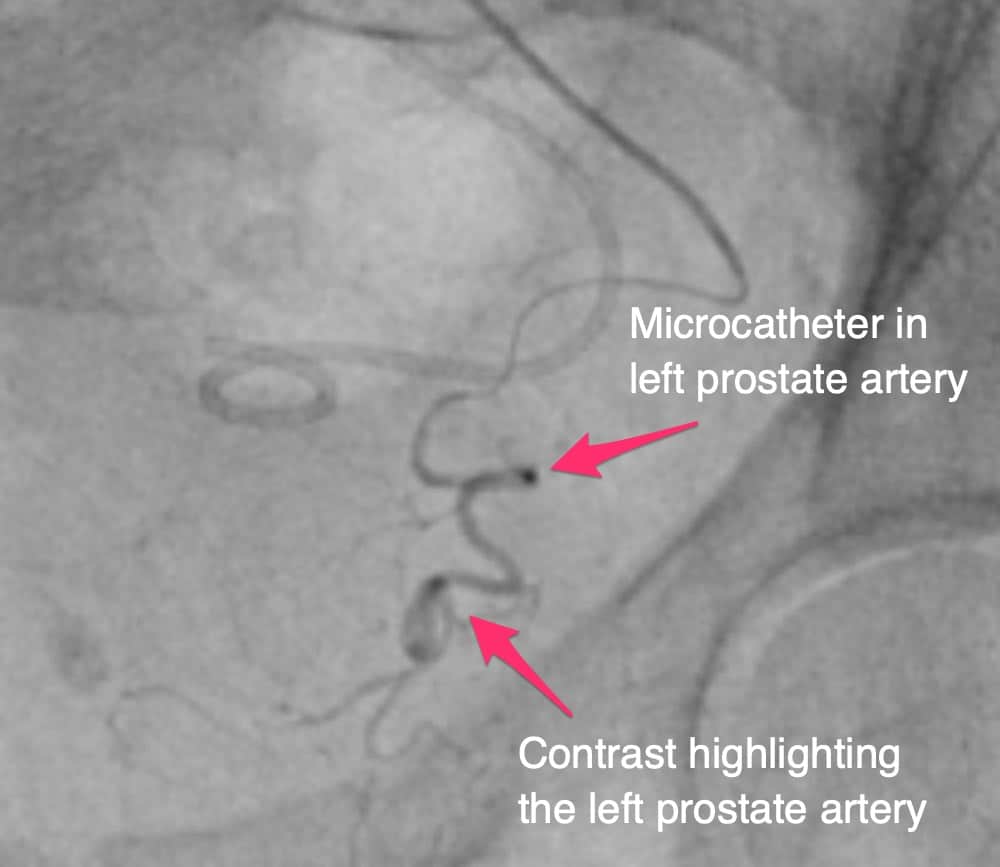
Prostatic Artery Embolization is a contemporary, image-guided procedure designed to reduce prostate volume and alleviate lower urinary tract symptoms caused by BPH. It involves the selective occlusion of prostatic arteries using embolic materials, typically calibrated microspheres, to induce ischemia and subsequent shrinkage of hyperplastic tissue. Since its initial clinical application in the early 2000s, PAE has been viewed as a minimally invasive alternative that preserves surrounding tissues and minimizes recovery time. Yet, the vascular anatomy of the pelvis and prostate presents unique challenges, which underpin many of the risks associated with the procedure. Recognizing these risks necessitates a thorough comprehension of pelvic vascular complexity.
The Landscape of Risks in Prostatic Artery Embolization

While PAE generally exhibits a favorable safety profile, the intimate vascular relationships within the pelvis predispose to certain complications. These risks can be broadly classified into vascular, non-vascular, and functional categories. To fully appreciate their impact, one must consider how anatomical variations, procedural techniques, and patient-specific factors interplay in risk manifestation. For example, inadvertent embolization of non-prostatic arteries can lead to ischemic damage in unintended tissues, raising questions about how pre-procedural planning can be optimized to prevent such mishaps.
Vascular Risks: Non-Target Embolization & Vascular Injury
One of the most significant concerns during PAE is non-target embolization, where embolic agents inadvertently occlude arteries supplying adjacent organs. Such mishaps may lead to ischemic injuries in tissues like the bladder, rectum, or penis. For instance, the prostatic arterial supply often shares common origins with the superior vesical artery and internal pudendal artery. If not carefully navigated, embolic particles can divert to these branches, jeopardizing their respective territories. Data indicate that the incidence of clinically significant non-target embolization remains low (< 2%), but when it occurs, what is its true clinical significance, and how is it best predicted or mitigated?
| Relevant Category | Substantive Data |
|---|---|
| Incidence of non-target embolization | Approximately 1.5-2% in large series; mostly minor, self-limiting ischemic events |
| Risk factors for non-target embolization | Anatomical variants, prior pelvic interventions, suboptimal imaging guidance |
| Mitigation strategies | Detailed pre-procedural vascular mapping, cone-beam CT, super-selective catheterization |
Vascular Injury and Hemorrhage
Vascular injury may manifest as arterial dissection or perforation, which, although uncommon (< 1%), can have serious consequences. Such injuries often result from aggressive catheter manipulation or challenging anatomy. Hemorrhagic complications, such as rectal bleeding, are typically minor but could escalate if not promptly addressed. An important question arises: what protocols should be established to promptly identify and manage vascular injuries during PAE to prevent escalation into more severe complications?
Non-Vascular Risks & Functional Complications
Beyond vascular injury, patients undergoing PAE can experience a range of other risks. These include urinary problems, infections, and functional deficits. Particularly concerning are transient or persistent urinary symptoms following the procedure, which may stem from ischemic edema or inflammation. Moreover, as PAE involves embolization of arteries near the bladder neck, is there a potential for impaired bladder function or erectile disturbances post-procedure? Evaluating this risk requires an understanding of pelvic neurovascular anatomy and how procedural alterations might impact these sensitive structures.
Infection and Post-Procedural Inflammation
The risk of infection post-PAE is relatively low (< 3%) but can be more serious when it occurs. Due to the embolic process inducing tissue ischemia, the prostate tissue becomes necrotic, which can serve as a nidus for bacterial growth. Adequate sterilization protocols, peri-procedural antibiotics, and patient selection are strategies to limit infections. So, could personalized risk assessment based on urinary tract microbiome or immunological status enhance preventative measures?
| Relevant Category | Substantive Data |
|---|---|
| Infection rate | Approximately 2.5-3% in large cohorts; mainly urinary tract infections |
| Prevention | Prophylactic antibiotics, sterile technique, patient education |
| Complications | Sepsis, abscess formation, persistent prostatitis in rare cases |
Other Considerations: Radiation & Contrast Risks
Performing PAE involves exposure to ionizing radiation during angiography. Although doses are generally within safe limits (< 5 Gy cumulatively), repeated procedures or complex anatomies can increase exposure. Contrast-induced nephropathy is another concern, especially in patients with pre-existing renal impairment. For example, in patients with chronic kidney disease (CKD), the risk of contrast nephropathy can be as high as 15-20%. These aspects invoke the question: how can procedural protocols be optimized to minimize these risks without compromising technical success?
Strategies for Risk Reduction in Imaging
Low-dose fluoroscopy protocols, the use of carbon dioxide angiography where feasible, and pre-procedural hydration are techniques to mitigate these concerns. But does the integration of newer imaging modalities, such as fusion imaging or contrast-enhanced ultrasound, hold promise for safer, radiation-sparing PAE? When evaluating patients with renal impairment, should alternative embolization techniques be considered to circumvent contrast use altogether?
| Relevant Category | Substantive Data |
|---|---|
| Radiation dose | Average fluoroscopy dose during PAE is 2-4 Gy; risk increases with procedure complexity |
| Contrast nephropathy incidence | In CKD patients, up to 15% risk; higher with dehydration or pre-existing risk factors |
| Preventive measures | Hydration, limiting contrast volume, alternative imaging techniques |
Patient Selection & Risk Management Strategies
Identifying optimal candidates for PAE involves weighing potential benefits against these risks. Factors such as prostate size, vascular anatomy, prior pelvic surgeries, and comorbid conditions like cardiovascular disease or renal impairment influence risk profiles. Should patient-specific anatomical mapping and risk stratification become routine to anticipate and prevent complications? Moreover, what role might pre-procedural planning software and multidisciplinary collaboration play in enhancing safety?
Informed Consent & Shared Decision-Making
Given the spectrum of risks, transparent communication with patients about potential complications is critical. Do comprehensive educational tools improve patient understanding, and does this, in turn, influence the choice of treatment? How can clinicians balance presenting statistical risks with individualized prognostic data to support shared decision-making?
Conclusion: Navigating the Balance Between Innovation and Risk
Prostatic Artery Embolization stands at the forefront of minimally invasive BPH management. Its potential to reduce dependence on surgical interventions is significant, yet acknowledging and understanding its common risks is essential for its safe integration into clinical practice. As technological advancements and procedural refinements continue, the focus must remain on patient-centered outcomes, risk mitigation, and evidence-based improvements. Which innovations or protocols will rise to prominence in minimizing risks while maximizing benefits? Are we on the cusp of a new standard that marries safety with efficacy in prostatic vascular interventions?
Key Points
- Non-target embolization remains the most prevalent risk, with precise imaging reducing incidence.
- Vascular injury, though rare, requires meticulous technique and prompt management strategies.
- Infection control protocols are vital, given the necrotic tissue response post-embolization.
- Radiation and contrast-related risks call for technological and procedural innovations to enhance safety.
- Enhanced pre-procedural planning and patient-specific risk assessment are central to minimizing adverse events.
What is the most common complication associated with PAE?
+The most common complication is non-target embolization, which can lead to ischemic injury in adjacent tissues, although currently it remains relatively rare.
How can the risk of non-target embolization be minimized?
+Utilizing detailed pre-procedural vascular mapping, advanced imaging techniques like cone-beam CT, and super-selective catheterization significantly reduce this risk by enhancing visualization and precision.
Are there long-term risks of vascular injury in PAE?
+While vascular injury such as dissection or perforation are rare, their occurrence underscores the need for skilled technique and careful navigation; long-term sequelae are uncommon when managed appropriately.