On an unseasonably crisp morning in downtown Chicago, Dr. Lisa Carter, a seasoned radiologist with over two decades of experience, paused momentarily amidst her bustling schedule. With a reverent glance at her imaging monitor, she reflected on a question frequently posed by patients and aspiring radiologists alike: Is ultrasound radiology truly the MRI of the diagnostic world? It’s a compelling query, rooted not merely in technical prowess but in the evolving landscape of medical imaging. To navigate this, one must delve into the nuances of diagnostic modalities, their historical trajectories, contemporary applications, and future prospects—unraveling whether ultrasound’s role rivals that of MRI in the grand orchestration of medical diagnostics.
Understanding Ultrasound Radiology: The Primer

Ultrasound radiology, also known as sonography, employs high-frequency sound waves to produce real-time images of internal body structures. It’s a modality distinguished by its safety profile—absolutely non-ionizing—and its versatility. The technique is predicated upon the principle that sound waves encounter tissues differently based on their composition, creating echogenic echoes that are translated into visual representations. Since its inception in the early 1950s, ultrasound has evolved from rudimentary devices to sophisticated systems capable of Doppler analysis, 3D imaging, and elastography.
Technological Evolution and Functional Capabilities
The advent of transducer miniaturization, digital signal processing, and computer-aided imaging has vastly expanded ultrasound’s diagnostic potential. Notably, Doppler ultrasound enables the assessment of blood flow dynamics, vital for cardiovascular and vascular diagnostics. Elastography extends this beyond mere anatomy, offering tissue stiffness measurements vital in oncology and fibrosis assessment. These advances have solidified ultrasound’s role as a bedside, immediate, and dynamic tool—attributes seldom matched by MRI’s more static imaging capability.
| Relevant Category | Substantive Data |
|---|---|
| Safety Profile | Non-ionizing radiation; suitable for frequent monitoring, especially in pregnancy |
| Diagnostic Speed | Real-time imaging allows immediate assessment, often in minutes |
| Cost-effectiveness | Substantially less expensive than MRI, accessible in most clinical settings |
Comparing Ultrasound to MRI: The Diagnostic Powerhouses

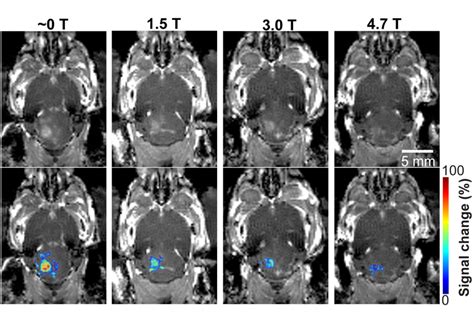
Magnetic Resonance Imaging emerged in the late 20th century as a revolutionary modality, offering unparalleled soft tissue contrast through the manipulation of magnetic fields and radiofrequency pulses. It excels in detailed visualization of brain, spinal cord, joints, and deep pelvic structures, often providing diagnostic insights that are unachievable with ultrasound. But does this mean ultrasound is merely complementary, or could it be considered the “MRI of the diagnostic world”?
Image Quality, Penetration, and Resolution
MRI’s superior soft tissue contrast and spatial resolution are unmatched, especially in intracranial pathology, musculoskeletal detail, and complex abdominal examinations. Ultrasound, however, is limited by its shallow depth of penetration—typically 12–20 cm depending on tissue density—and operator dependency introduces variability in image quality. Yet, in accessible and dynamic contexts, ultrasound produces excellent resolution for superficial structures and is highly effective for rapid assessments.
| Relevant Category | Substantive Data |
|---|---|
| Soft Tissue Contrast | MRI provides 3D imaging with excellent differentiation of tissue types; ultrasound offers less contrast but high-resolution images of superficial tissues |
| Operational Environment | MRI requires a dedicated facility and is sensitive to patient movement; ultrasound is portable and can be used at the bedside or in outpatient clinics |
| Procedure Duration | MRI examinations may last 30–60 minutes; ultrasound is often completed within 15–30 minutes or less |
Clinical Applications and Domain-Specific Advantages
Ultrasound’s clinical utility spans a broad spectrum—from obstetrics and gynecology to cardiology, emergency medicine, and musculoskeletal diagnostics. Its real-time imaging capability facilitates procedures like biopsies, drainages, and guided interventions, often reducing the need for more invasive or costly imaging. Conversely, MRI’s role is pivotal in neurology, oncology, and complex spine and joint disorders—domains where its superior contrast and multispectral imaging provide definitive answers impossible with ultrasound.
Obstetrics and Gynecology: Ultrasound’s Forte
Ultrasound remains the cornerstone for prenatal monitoring, fetal anomaly screening, and ovarian or uterine pathology evaluation due to its safety profile and portability. MRI complements this by providing detailed soft tissue contrasts when ultrasound findings are inconclusive, such as in cases of complex pelvic masses or fetal CNS anomalies.
Cardiovascular and Emergency Medicine
The immediacy of transthoracic echocardiography allows cardiac function assessment at the bedside, critical in acute settings like heart failure or trauma. MRI, with its exquisite detail of myocardial tissue characterization, fills in the gaps for chronic cardiomyopathies or myocarditis, where tissue composition is vital to diagnosis.
| Relevant Category | Substantive Data |
|---|---|
| Procedural Guidance | Ultrasound guides real-time interventions, decreasing complication rates |
| Deep Tissue Analysis | MRI excels at evaluating deep-seated or complex soft tissue abnormalities |
Future Perspectives: AI, Fusion Imaging, and Beyond
The frontiers of diagnostic imaging are increasingly intertwining, with artificial intelligence (AI) and machine learning revolutionizing image acquisition and interpretation. Ultrasound, already benefiting from AI-enhanced image stabilization and automated measurements, is poised to gain from real-time diagnostic algorithms. Similarly, MRI’s volumetric and spectral data are being integrated with AI for predictive analytics, personalized treatment planning, and molecular imaging.
Fusion Imaging: Merging Modalities for Maximized Insight
The development of hybrid imaging systems, combining ultrasound and MRI, aims to leverage the strengths of both modalities. Fusion imaging is particularly promising in oncological interventions and complex vascular procedures, allowing clinicians to navigate precisely during minimally invasive therapies.
| Relevant Category | Substantive Data |
|---|---|
| AI Integration | AI algorithms improve image quality and diagnostic accuracy in ultrasound and MRI |
| Fusion Technologies | Devices that synchronize real-time ultrasound with pre-acquired MRI enhance procedural safety and effectiveness |
Concluding Thoughts: The Paradigm of Diagnostic Modalities
The contemplation of whether ultrasound radiology is the MRI of the diagnostic domain highlights more than a simple comparison of imaging qualities. It underscores the evolving understanding that no single modality holds definitive supremacy; rather, an integrated approach, tailored to clinical question, patient profile, and resource availability, epitomizes best practice. Ultrasound’s agility, safety, and cost-effectiveness make it indispensable in diverse settings, while MRI’s unmatched soft tissue contrast renders it irreplaceable in specific, complex diagnostics.
Ultimately, the analogy might be less about competition and more about collaboration—each modality, with its unique strengths and limitations, contributing to a richer, more nuanced tapestry of diagnostic intelligence. As technological advancements continue to blur traditional boundaries, clinicians stand to benefit from a future where multimodal imaging becomes seamlessly integrated, empowering precise, timely, and patient-centered care.
Can ultrasound fully replace MRI in soft tissue diagnostics?
+While ultrasound is excellent for superficial and real-time imaging, it cannot fully replace MRI for deep or complex soft tissue structures that require high contrast resolution. Instead, the two modalities often complement each other based on clinical needs.
What are the main limitations of ultrasound compared to MRI?
+Ultrasound faces limitations in depth penetration, operator dependency, and acoustic window availability. It also provides less tissue contrast than MRI, especially in deep-seated or complex anatomical regions.
How is AI influencing the future of ultrasound and MRI?
+AI enhances image quality, automates measurements, and facilitates real-time diagnosis in ultrasound. In MRI, AI assists in image reconstruction, spectral analysis, and predictive analytics, promising a more integrated and intelligent imaging ecosystem.
