In the realm of medical imaging, particularly ultrasonography, the characterization of lesions based on their echogenicity patterns plays a pivotal role in guiding diagnostic pathways. Among these, hypoechoic lesions—those that appear darker relative to surrounding tissues—pose both a challenge and an opportunity for clinicians and radiologists aiming to discriminate benign from malignant processes. What intrinsic features define hypoechoic lesions, and by what imaging characteristics can we enhance diagnostic accuracy? More fundamentally, how does understanding these features influence clinical decision-making, patient management, and prognostic assessments? The pursuit of these questions leads us into a deep exploration of the imaging intricacies, histopathological correlations, and evolving diagnostic algorithms associated with hypoechoic lesions across various organ systems.
Fundamental Concept of Hypoechoic Lesions in Ultrasonography
To appreciate the significance of hypoechoic lesions, one must first understand the basic principles of ultrasound imaging. How do the physical properties of tissues influence their ultrasound appearance? The echogenicity of a lesion is primarily determined by its acoustic impedance relative to adjacent tissues, with hypoechoic lesions exhibiting lower impedance, thus absorbing or transmitting more ultrasound waves than reflecting them back. This results in a darker appearance on the ultrasound image. But does a hypoechoic pattern necessarily imply pathology? Or can it also represent normal or benign variants? These questions underpin the importance of context and additional imaging features in interpretation.
The Spectrum of Echogenicity and Its Diagnostic Implications
When classifying lesions based on echogenicity, radiologists often consider terms such as anechoic, hypoechoic, isoechoic, hyperechoic, and complex. Hypoechoic signifies a lesion darker than surrounding tissue but may encompass a broad spectrum including cysts, neoplasms, inflammation, and even some benign masses. Isn’t it fascinating how similar ultrasound appearances can correspond to such diverse histopathological entities? How then can we stratify risk or probability of malignancy purely from image pattern? This is where additional imaging features—margins, internal architecture, vascularity—become critical.
| Relevant Category | Substantive Data |
|---|---|
| Prevalence in Organs | In thyroid imaging, hypoechoic nodules constitute approximately 70-80% of malignant tumors, whereas in the liver, they often correspond to cysts or metastases. |
| Ultrasound Features | Margins (well-defined vs. irregular), internal architecture (homogeneous vs. heterogeneous), and presence of calcifications influence diagnostic suspicion. |
| Biopsy Correlation | Malignant hypoechoic lesions often show increased vascularity, microcalcifications, and invasive borders, confirmed through histopathology. |
Imaging Features of Hypoechoic Lesions in Various Organ Systems
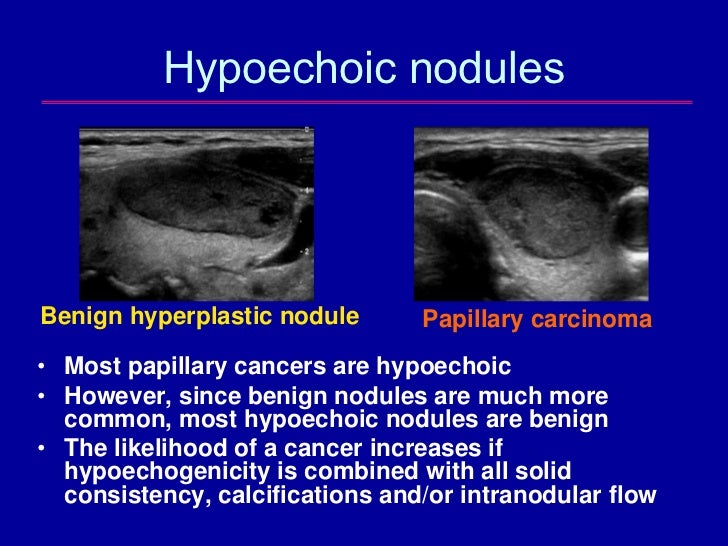
Thyroid Nodules and Risk Stratification
The thyroid gland offers a classic example where hypoechoic nodules warrant healthful scrutiny. Are hypoechogenicity and irregular margins sufficient to warrant suspicion? Likely not—these features are part of composite risk models like TI-RADS, which integrate shape, margins, echogenicity, composition, and echogenic foci. How does the presence of microcalcifications within a hypoechoic nodule modify the pre-test probability of malignancy? Evidence suggests that microcalcifications significantly elevate the suspicion index, echoing the histopathological importance of papillary carcinoma indicators.
Liver Lesions: Benign or Malignant?
In hepatic imaging, hypoechoic lesions are common, yet their differential diagnosis spans simple cysts, hemangiomas, metastases, and hepatocellular carcinoma. How do Doppler features and contrast-enhanced phases assist in narrowing this differential? For instance, hypervascularity in arterial phases with washout during portal venous phases hints at malignancy. Can contrast-enhanced ultrasound improve early detection and characterization? Current data supports its utility in differentiating these lesions, especially when MRI contrast is contraindicated or unavailable.
Breast Lesions
In breast ultrasonography, hypoechoic masses with irregular margins and spiculations raise concern for carcinoma. Yet, some benign fibroadenomas also exhibit hypoechogenicity. How does lesion stiffness measured via elastography contribute? Higher stiffness correlates with malignancy, adding another layer of specificity. Is it possible that a combination of echogenicity and mechanical assessment could refine our diagnostic confidence?
Key Points
- Understanding morphological features such as borders, internal architecture, and vascularity enhances radionavigation of hypoechoic lesions.
- Multimodal imaging, including contrast-enhanced ultrasound and elastography, provides critical functional and mechanical data, improving specificity.
- Histopathological correlation remains the gold standard, but imaging can guide biopsy decisions effectively.
- Technological advances continue to refine the interpretive accuracy of hypoechoic lesion assessment across organ systems.
- Risk stratification models help integrate multiple imaging features, leading to intelligent clinical pathways.
Diagnostic Challenges and Limitations
Are there pitfalls or overlaps that could mislead even the experienced eye? Certainly, benign entities such as colloid nodules, hemorrhagic cysts, or post-inflammatory scars may mimic malignant features. Conversely, some malignancies might appear deceptively benign. How can we balance reliance on ultrasound with complementary modalities? The combination of imaging, clinical context, and, when necessary, tissue diagnosis forms a holistic approach. Do emerging artificial intelligence tools hold promise for reducing observer variability? Preliminary studies suggest potential, but are they yet ready for routine clinical integration?
Emerging Technologies and Future Directions in Imaging of Hypoechoic Lesions
Advancements such as shear wave elastography, contrast-enhanced harmonic imaging, and quantitative sonoelastography are at the forefront of refining lesion assessment. How do these tools help elucidate tissue stiffness, perfusion, and microvascular architecture? Might they help overcome the current limitations of subjective interpretation? Furthermore, integrating machine learning algorithms trained on large datasets could revolutionize risk prediction and diagnostic accuracy. What barriers—technical, ethical, or infrastructural—stand in the way of widespread adoption?
What are the key ultrasound features that suggest malignancy in hypoechoic lesions?
+Irregular margins, microcalcifications, taller-than-wide shape, increased vascularity, and heterogeneity within hypoechoic lesions are suspicious features. Combining these features increases diagnostic confidence.
How does contrast-enhanced ultrasound improve lesion characterization?
+It assesses lesion perfusion patterns, highlighting abnormal vascularity and washout characteristics that are typical of malignancies, thereby refining differential diagnosis beyond traditional gray-scale imaging.
Can artificial intelligence assist in diagnosing hypoechoic lesions?
+AI algorithms can analyze large imaging datasets to recognize complex patterns, potentially increasing diagnostic accuracy and reducing observer variability, but require extensive validation before routine use.