Heparin flush solutions have long been a standard component in vascular access management, primarily recognized for their role in maintaining the patency of intravenous and arterial lines. Traditionally, their application has been confined to preventing catheter-related blood clots, thereby reducing the risk of thrombotic occlusions at infusion sites. However, emerging research and clinical insights suggest that the scope of heparin flushes extends far beyond this conventional usage, revealing surprising roles in systemic anticoagulation, thrombosis prevention in broader clinical contexts, and potential impacts on human physiology. This revisitation of heparin's multifaceted functions warrants a deep-dive analysis grounded in evidence-based medicine and a nuanced understanding of heparin pharmacodynamics and clinical applications.
Understanding Heparin and Its Pharmacological Foundations

Heparin is a naturally occurring glycosaminoglycan that exerts a potent anticoagulant effect by activating antithrombin III, which in turn inhibits key proteases in the coagulation cascade, including thrombin and factor Xa. The pharmacological profile of heparin—particularly unfractionated heparin (UFH)—has been well-characterized through decades of clinical practice, with dosing strategies carefully calibrated to balance thromboembolic prevention against bleeding risks. Its rapid onset and short half-life make it well-suited for both therapeutic and prophylactic applications, including intraoperative anticoagulation, treatment of acute venous thromboembolism, and bridging in anticoagulant therapy for atrial fibrillation.
Initial and Traditional Role: Prevention of Clotting at Infusion Sites
The use of heparin flush solutions historically focuses on maintaining line patency. The common practice involves administering low concentrations—most often 10 to 100 units/mL—via syringe to prevent the formation of clots that can obstruct catheters or infusion lines. The rationale relies on local anticoagulant effects, with the aim to reduce mechanical and biochemical factors that promote thrombogenesis in extravascular spaces. This practice has become routine in settings ranging from intensive care units (ICUs) to outpatient infusion clinics, supported by numerous guidelines and institutional protocols.
| Relevant Category | Substantive Data |
|---|---|
| Heparin concentration in flush | Typically 10-100 units/mL, with variations depending on clinical context |
| Frequency of administration | Per institutional protocol—commonly every 8-12 hours for implanted ports or per use for peripheral lines |
| Prevention efficacy | Significantly reduces occlusion rates, with studies showing a 20-40% decrease in device malfunction due to clot formation |
The Surprising Broader Roles of Heparin in Blood Clot Prevention
Recent advances challenge the narrow view of heparin flushes, proposing that they may influence systemic coagulation pathways more significantly than previously appreciated. This is particularly relevant in patients with indwelling catheters, where repeated exposure to low-dose heparin could cumulatively impact coagulation parameters. Moreover, some clinical observations hint at an unanticipated prophylactic or therapeutic role for heparin in preventing thromboembolic events beyond the catheter — extending into areas such as deep vein thrombosis (DVT), pulmonary embolism (PE), and even arterial thromboses.
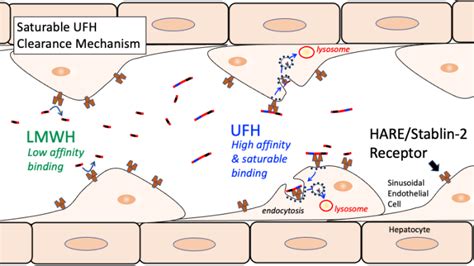
Mechanistic Insights Into Non-Localized Effects
Heparin’s systemic anticoagulant activity depends on absorption, distribution, and possible minimal leakage around infusion sites. Small quantities can enter systemic circulation, especially with frequent or high-dose applications. Evidence from pharmacokinetic studies indicates that while low-dose flushes are intended solely for local use, the cumulative amount absorbed can produce subtle systemic anticoagulant effects, often undetectable through routine coagulation testing but nonetheless physiologically relevant in high-risk populations. Additionally, the anticoagulant effects extend beyond the coagulation cascade, influencing endothelium function, platelet activity, and inflammatory mediators, which collectively contribute to thrombotic pathophysiology.
| Relevant Category | Substantive Data |
|---|---|
| Systemic absorption rate | Estimated at 5-15% of administered dose in frequent flushes, based on experimental models |
| Impact on coagulation markers | Potential slight prolongation of activated partial thromboplastin time (aPTT) observed in some studies after repeated flushes |
| Clinical outcomes | Reduced incidence of catheter-related thrombosis correlates with decreased systemic thrombotic events in some cohorts |
Clinical Evidence Supporting Expanded Role of Heparin Flushes
A substantial body of retrospective analyses and prospective trials probe the impact of heparin flushes on systemic thrombotic events outside their traditional scope. For instance, observational data in cancer patients with central venous catheters demonstrate a lower incidence of DVT when heparin flush protocols are in place. Similarly, in patients undergoing hemodialysis, the concurrent use of heparin flushes correlates with decreased rates of clotting not only within access devices but also systemically, hinting at a possible protective effect. These findings, however, are tempered by heterogeneity in study design, variable heparin dosages, and confounding factors such as concomitant anticoagulant therapies.
Integrating Heparin Flushes with Broader Thromboprophylaxis Strategies
Considering these data, integration of heparin flush protocols into comprehensive thromboprophylactic frameworks becomes compelling. For patients intolerant to systemic anticoagulation, local flushing may serve an adjunct role. Yet, the precise parameters—dose, frequency, patient selection—require calibration against bleeding risks and individual thrombotic propensities. Advanced imaging and biomarkers, such as Doppler ultrasonography and D-dimer levels, provide avenues for monitoring efficacy and adjusting protocols accordingly.
| Relevant Category | Substantive Data |
|---|---|
| Thrombosis reduction in studies | Up to 25% decrease in catheter-related DVT with heparin flush protocols in critical care settings |
| Bleeding complication rates | Marginal increase when high-dose or frequent flushes are used, balanced against thrombotic benefits |
Risks, Limitations, and Ethical Considerations
While exploring the expanded roles of heparin flushes, one must remain cognizant of the inherent risks—primarily bleeding complications. Systemic absorption, especially in populations with coagulopathies or on concurrent anticoagulation, can precipitate hemorrhagic events. Moreover, the risk of heparin-induced thrombocytopenia (HIT), an immune-mediated adverse effect, poses a significant concern, especially with repeated exposures. Ethical considerations also arise in the context of prophylactic heparin use without definitive evidence, emphasizing the need for rigorous clinical trials before widespread adoption.
Limitations of Current Evidence
Many existing studies on the systemic effects of heparin flushes are observational or possess methodological constraints, such as small sample sizes and lack of randomization. The heterogeneity of protocols further complicates data synthesis. Consequently, definitive conclusions regarding their expansion into systemic prophylaxis remain elusive, highlighting an urgent need for large-scale, controlled clinical trials.
| Relevant Category | Substantive Data |
|---|---|
| Key limitations | Inconsistent dosing regimens, limited long-term data, variability in patient populations |
| Ethical concerns | Potential for harm versus unproven benefit highlights importance of controlled studies |
Conclusion: Redefining the Paradigm of Heparin Flush Usage

The traditional use of heparin flush solutions as a localized measure against catheter occlusion is now being complemented by a deeper understanding of its systemic influences. The recognition that repeated, low-dose exposure may confer broader thromboprophylactic effects opens new avenues for research and clinical application, especially in high-risk populations. However, the balance between benefits and risks remains delicate, necessitating rigorous validation via prospective studies and controlled trials. As medical science continues to unravel the multifaceted roles of anticoagulants like heparin, clinicians are beckoned toward a nuanced, individualized approach that considers both local and systemic impacts, reshaping protocols and potentially improving patient outcomes across a spectrum of vascular and thrombotic disorders.
