When Dr. Emily Carter stepped into her clinical practice in downtown Chicago, she was driven by a singular purpose: transforming lives through advanced cardiovascular surgery. Yet, amidst the cutting-edge technology and expert team, she encountered often-unspoken barriers—one of them being the staggering costs associated with heart transplants. Her patients, many of whom faced the brink of life and death, often found themselves paralyzed by financial uncertainty, wondering how they would afford such a life-saving procedure. This personal experience sparked her curiosity and passion to explore the multifaceted dimensions of heart transplant costs—an often underappreciated facet of complex healthcare delivery.
Comprehensive Breakdown of Heart Transplant Cost Components

The expenses tied to heart transplantation are a complex mosaic, influenced by numerous intersecting factors ranging from medical procedure intricacies to regional economic variations. For patients and policymakers alike, understanding these financial dimensions is crucial for informed planning and resource allocation. The total cost of a heart transplant typically encompasses several core elements, each driven by specific technical, logistical, and economic variables.
Pre-Transplant Evaluation and Preparation
Before a patient can be considered for transplantation, a rigorous evaluation process is necessary to determine suitability, involving a battery of diagnostic tests, imaging, psychological assessments, and extensive consultations. The costs for these assessments are substantial, often averaging between 30,000 and 50,000 in the United States, depending on the facility and geographic location. These evaluations are essential to identify potential contraindications, optimize candidate health, and reduce postoperative complications.
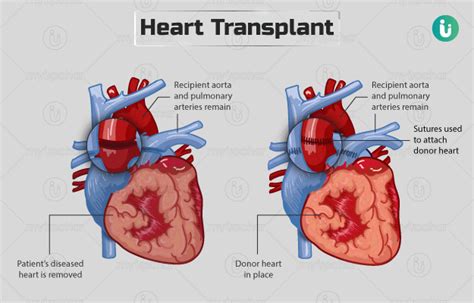
Surgical Procedure and Immediate Postoperative Care
The surgical heart transplant itself is a highly specialized operation that requires a proficient team of cardiothoracic surgeons, anesthesiologists, and perioperative nurses. In the US, the direct surgical costs—covering operating room, surgical supplies, medications, and immediate postoperative intensive care—range from 800,000 to 1 million. Notably, these figures can vary significantly in different countries, influenced by labor costs, technology availability, and healthcare system efficiency.
| Relevant Category | Substantive Data |
|---|---|
| Surgical Cost | $800,000–$1 million in the US |
| Evaluation Expense | $30,000–$50,000 pre-surgery |
| Postoperative Care | Typically $100,000–$300,000 for the first year |

Post-Transplant Medication and Long-Term Management
The success of a heart transplant depends heavily on lifelong immunosuppressive therapy and regular monitoring to prevent rejection, infections, and other complications. These medications alone can amount to 20,000 to 30,000 annually. The financial burden extends over the patient’s lifetime, with cumulative costs that can surpass $1 million—yet this investment is vital for long-term graft survival.
Additional Expenses: Logistics, Infrastructure, and Indirect Costs
Beyond direct medical costs, logistical expenses include donor organ procurement, transportation logistics, and infrastructure support systems. The procurement process, involving coordination among multiple hospitals, tissue banks, and transportation services, often adds an estimated 50,000–100,000 per transplant case. Additionally, indirect costs—like loss of productivity, caregiver burden, and long-term rehabilitation—must be factored into the overall economic impact.
Influence of Regional and Institutional Factors on Transplant Costs

Regional disparities substantially influence the financial landscape. For example, in countries with publicly funded healthcare systems, such as the UK’s NHS, the per-case expense may be significantly lower due to government-negotiated drug prices, centralized procurement, and standardized protocols. Conversely, private healthcare markets, especially in North America, often reflect higher prices driven by administrative overheads, higher staffing costs, and technological investments.
Impact of Technological Advancements and Policy Interventions
Emerging innovations—such as robotic-assisted transplantation, improved immunosuppressive therapies, and telemedicine-based follow-up—hold promise for reducing costs and improving outcomes over time. Policy interventions, focusing on organ donation campaigns and national registries, can also influence overall costs by increasing organ availability, thereby decreasing wait times and related complications.
| Related Entity | Impact on Cost |
|---|---|
| Technology Innovation | Potential cost reductions through minimally invasive techniques |
| Organ Donation Programs | Reduced waitlist mortality, fewer emergency procedures |
| Healthcare Policies | Standardization may decrease variability in costs |
Financial Planning for Patients and Healthcare Systems
Given the substantial costs associated with heart transplantation, meticulous financial planning is predicated on early assessment of expenses and comprehensive coverage strategies. Patients must navigate insurance complexities, often balancing Medicare, Medicaid, private insurance, and out-of-pocket payments. On a systemic level, health authorities face the challenge of allocating resources efficiently to maximize survival rates while maintaining fiscal sustainability.
Insurance Coverage and Out-of-Pocket Expenses
In the U.S., insurance plans often cover a significant portion of transplant costs, yet patients may still face deductibles, copayments, and coverage limits. For example, Medicare covers heart transplants for individuals under 65 with end-stage heart failure, covering around 80% of approved expenses; however, supplementary coverage is frequently necessary for additional costs. Out-of-pocket expenses can reach tens of thousands of dollars, creating barriers for uninsured or underinsured populations.
Financial Assistance Programs and Policy Initiatives
Numerous charitable organizations and government initiatives aim to mitigate financial barriers. The National Foundation for Transplants and similar entities provide grants for medication, transportation, and housing. Long-term sustainability hinges on policy reforms that expand access, such as increasing Medicaid coverage or establishing more comprehensive national transplant funding schemes.
Economic Models and Cost-Effectiveness Analyses
Cost-effectiveness analyses (CEA) are instrumental in evaluating the long-term value of heart transplants. A 2021 study published in the Journal of Heart and Lung Transplantation concluded that, despite high initial costs, the quality-adjusted life year (QALY) gained justifies transplantation, with an average cost per QALY around $50,000—considered within acceptable thresholds for life-saving interventions.
Future Perspectives: Innovations and Financial Implications
Looking ahead, advancements such as bioengineered hearts and xenotransplantation from genetically modified donors hint at a future where transplant costs may decrease through technological breakthroughs and increased organ availability. Yet, these innovations also introduce new cost structures related to research, regulation, and infrastructure adaptation. The integration of artificial intelligence in donor-recipient matching presents opportunities for optimizing outcomes and minimizing expenditure through precise, data-driven decision-making.
Emerging Technologies and Their Potential Cost Impact
Laboratory efforts in tissue engineering aim to produce personalized organs, potentially eliminating the donor shortage and reducing the costs associated with organ procurement logistics. Similarly, ex vivo organ preservation techniques extend preservation times, allowing better matching and reducing wastage—translating into economic efficiencies.
| Technology | Expected Cost Implication |
|---|---|
| Bioengineered Hearts | High initial R&D costs expected to decrease with scale and efficiency |
| Xenotransplantation | Cost of genetic modification and sterilization balanced against increased availability |
| AI-Assisted Matching | Potential to lower overall healthcare costs through optimized resource use |
What are the main factors influencing heart transplant costs?
+Factors include preoperative evaluation expenses, surgical procedure costs, postoperative medication, infrastructure, regional economic variations, and long-term management needs. Each element significantly shapes the overall financial landscape.
How can patients prepare financially for a heart transplant?
+Patients should review their insurance coverage, explore assistance programs, and consult financial counselors. Early planning ensures they understand potential out-of-pocket expenses and available resources for long-term management.
Are technological advances likely to reduce heart transplant costs?
+Emerging innovations like bioengineering and AI-driven matching hold promise for cost reductions by improving organ availability, reducing complications, and enhancing procedural efficiencies, although initial investments are substantial.