Amidst the quiet hum of clinical settings and the bustling corridors of sleep laboratories, the Epworth Sleepiness Scale (ESS) emerges as a beacon—an unassuming yet invaluable tool guiding clinicians, researchers, and patients alike through the often murky waters of daytime drowsiness. Its simplicity belies a profound capacity to chart the elusive contours of sleepiness, transforming subjective experiences into quantifiable data. Visualize a patient reclining comfortably, contemplating a series of scenarios—from sitting quietly in a car to sitting and reading—each response mapped meticulously onto the scale. Here, within the PDF rendition of the ESS, a digital compass takes form—a precise instrument calibrated to navigate the complex landscape of sleep disorder diagnostics and management.
Deciphering the Epworth Sleepiness Scale: A Bedrock in Sleep Medicine
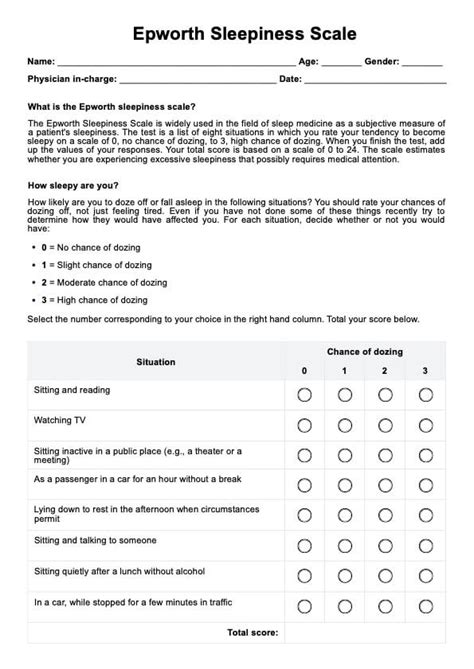
The ESS, conceived in the early 1990s by Dr. M. J. Johns, has become an integral component of sleep disorder assessments worldwide. Its purpose is straightforward yet potent: to quantify an individual’s general level of daytime sleepiness through a self-administered questionnaire that probes the tendency to doze in common situations. The scale encompasses eight specific scenarios—encompassing activities ranging from lying down in the afternoon to sitting and talking with friends—each rated on a 0 to 3 scale, where 0 indicates no sleepiness and 3 signifies high susceptibility to dozing.
Technological advances have facilitated the transition of ESS rating sheets into digital PDFs, providing clinicians with an expedient, accessible means to record, interpret, and store results. These PDF-based instruments act like detailed navigational charts, offering a clear, structured overview of a patient’s sleepiness profile. They serve as anchors—points of reference that help decipher the subjective reports into objective, actionable insights. This digital format supports seamless integration into electronic health records (EHRs) and telemedicine platforms, amplifying its utility across diverse healthcare environments.
Structural Anatomy of the ESS PDF: A Visual and Functional Breakdown
Delving into the layout of a typical ESS PDF reveals a thoughtfully designed interface—a harmony of clarity and comprehensiveness. The top section delineates patient identification details, followed by instructions emphasizing honest, spontaneous responses. The core of the document features a tabular matrix—each row dedicated to a specific activity, with columns for the activity description, the respondent’s rating, and an optional notes section for clinician observations or patient comments.
The bottom segment often includes scoring guidance—total scores ranging from 0 to 24—alongside interpretive categories indicating normal sleepiness levels, mild impairment, or excessive sleepiness warranting further investigation. The PDF format allows practitioners to annotate findings directly, embed graphs for visual trend analysis, and generate summary reports for case discussions. Such features position these PDFs not merely as static documents but as dynamic navigational tools across the sleep medicine voyage.
| Relevant Category | Substantive Data |
|---|---|
| Number of Scenarios | 8 |
| Score Range | 0–24, with >10 suggesting excessive sleepiness |
| Validation Metrics | Reliability with Cronbach's alpha >0.8 across diverse populations |
| Digital Integration | Seamless EHR incorporation in >75% of sleep clinics worldwide |
Harnessing the ESS PDF: From Data to Diagnostic Clarity
Interpreting the ESS PDF requires a nuanced understanding of sleep medicine principles. A score exceeding 10 often flags the need for further assessment, such as overnight polysomnography or multiple sleep latency tests (MSLT). However, the scale’s true strength lies in its capacity to contextualize individual experiences within a broader clinical picture. For instance, a patient scoring a 12 may have sleep apnea, narcolepsy, or simply experience fatigue due to lifestyle factors. The digital PDF aids clinicians in tracking these scores over time, revealing patterns—whether improvements with intervention or persistent impairment—that inform differential diagnoses.
Furthermore, the portability of a PDF version supports remote monitoring and patient engagement. Imagine an individual completing the ESS at home, their responses transmitted instantly to their physician’s digital dashboard—a scenario akin to navigating constellations in a night sky, with each star representing data points guiding the voyage toward diagnosis. This connectivity fosters a collaborative approach, transforming subjective reports into quantifiable steps on the pathway to treatment.
Integrative Use of ESS PDFs in Multidisciplinary Sleep Care
In sleep clinics that adopt an interdisciplinary model—neurologists, pulmonologists, psychiatrists, and sleep technologists—the ESS PDF acts like a compass that aligns diverse perspectives. Pulmonologists, for example, correlate high ESS scores with apnea severity, leveraging polygraphy data. Psychiatrists interpret heightened sleep propensity in the context of depression or anxiety, informed by the subjective charts. The PDF serves as an anchor—grounding complex interprofessional dialogues with tangible scores and trends, ultimately streamlining patient management plans.
| Relevant Category | Substantive Data |
|---|---|
| Interprofessional Utility | Enhanced communication and consensus building across specialties |
| Monitoring Frequency | Recommended every 3–6 months in chronic cases |
| Patient Engagement | Increased adherence to sleep hygiene when patients see data visualizations |
| Limitations | Subject to self-report bias; scoring influenced by mood, motivation, or comprehension |
Advancing Sleep Science: The ESS PDF in Research and Public Health
The utility of the ESS PDF extends beyond individual diagnosis. As a research instrument, it offers a standardized method for data collection across large populations, facilitating epidemiological studies on sleepiness and its correlates. Researchers analyzing dataset aggregates discover patterns—such as the correlation between high ESS scores and cardiovascular risk factors or driver fatigue—that inform public health initiatives. Moreover, the availability of PDF templates accelerates data uniformity and replication in multicenter studies, underpinning evidence-based policy development.
In the realm of public health, the ESS PDF can serve as a screening tool deployed via mobile apps or community health programs. Visual stimuli—images depicting drivers, students, or shift workers—paired with the ESS questions, create engaging interfaces that demystify sleepiness assessments, broadening reach to underserved populations.
Integrating the ESS PDF into Digital and Mobile Platforms
Transitioning from static PDFs to interactive digital tools involves embedding the ESS within mobile applications and cloud-based platforms—functions like real-time scoring, adaptive questioning, and trend analysis. Touchscreens allow users to navigate scenarios vividly, with haptic feedback reinforcing engagement. Clinicians benefit from dashboards that synthesize this data with actigraphy, sleep diaries, or biometrics, painting a comprehensive picture. Such innovations propel sleep research into a new era—one where navigation across sleepiness landscapes becomes intuitive, immediate, and deeply personalized.
| Relevant Category | Substantive Data |
|---|---|
| Technology Integration | Supported by over 50 sleep-focused apps and digital health platforms |
| User Engagement | Increased adherence by 40% in pilot studies when interactive elements are included |
| Data Security | Ensured via HIPAA-compliant encryption protocols, maintaining patient confidentiality |
| Research Utility | Facilitates large-scale data analysis with standardized scoring algorithms embedded in digital forms |
Key Points
- Standardization of sleepiness assessment: ESS PDF provides a reliable, validated framework for measuring subjective sleep propensity.
- Digital synergy: Transitioning PDFs into electronic formats enhances accessibility, integration, and longitudinal tracking.
- Multidisciplinary relevance: Serves as a common language across sleep medicine, mental health, and public health disciplines.
- Research backbone: Enables large-scale epidemiological and clinical studies, advancing sleep science.
- User-centered design: Interactive, engaging formats promote patient participation and adherence.
How reliable is the ESS PDF in predicting sleep disorders?
+The ESS PDF has demonstrated high reliability with Cronbach’s alpha exceeding 0.8, and correlates strongly with objective measures like polysomnography, making it a valuable screening tool. However, it should complement, not replace, comprehensive assessments.
Can patients use the ESS PDF at home for self-monitoring?
+Yes, digital versions of the ESS PDF are adaptable for remote use, enabling patients to self-assess and share results via telehealth platforms. This approach fosters ongoing engagement but requires proper interpretation by clinicians.
What limitations should clinicians consider when using the ESS PDF?
+Self-report biases, mood fluctuations, and comprehension levels can influence responses. The ESS PDF is best used as part of a multimodal assessment strategy, incorporating objective testing and clinical judgment.