As a gateway to some of the most intricate and delicate structures within the human skull, the temporal bone remains a subject of perpetual fascination among radiologists, otolaryngologists, and neurosurgeons alike. This complex bone, residing at the side and base of each skull, houses vital components like the cochlea, vestibular structures, and the middle and inner ear. Its anatomical intricacies, combined with the subtle variations in pathology and anatomy discernible through computed tomography (CT), render it a compelling field of study that bridges radiological precision with surgical nuance. To truly appreciate the marvels of the temporal bone, one must first understand its multifaceted structure, evolutionary background, and the technological advancements that illuminate its secrets on imaging.
The Complex Anatomy of the Temporal Bone: A Detailed Canvas

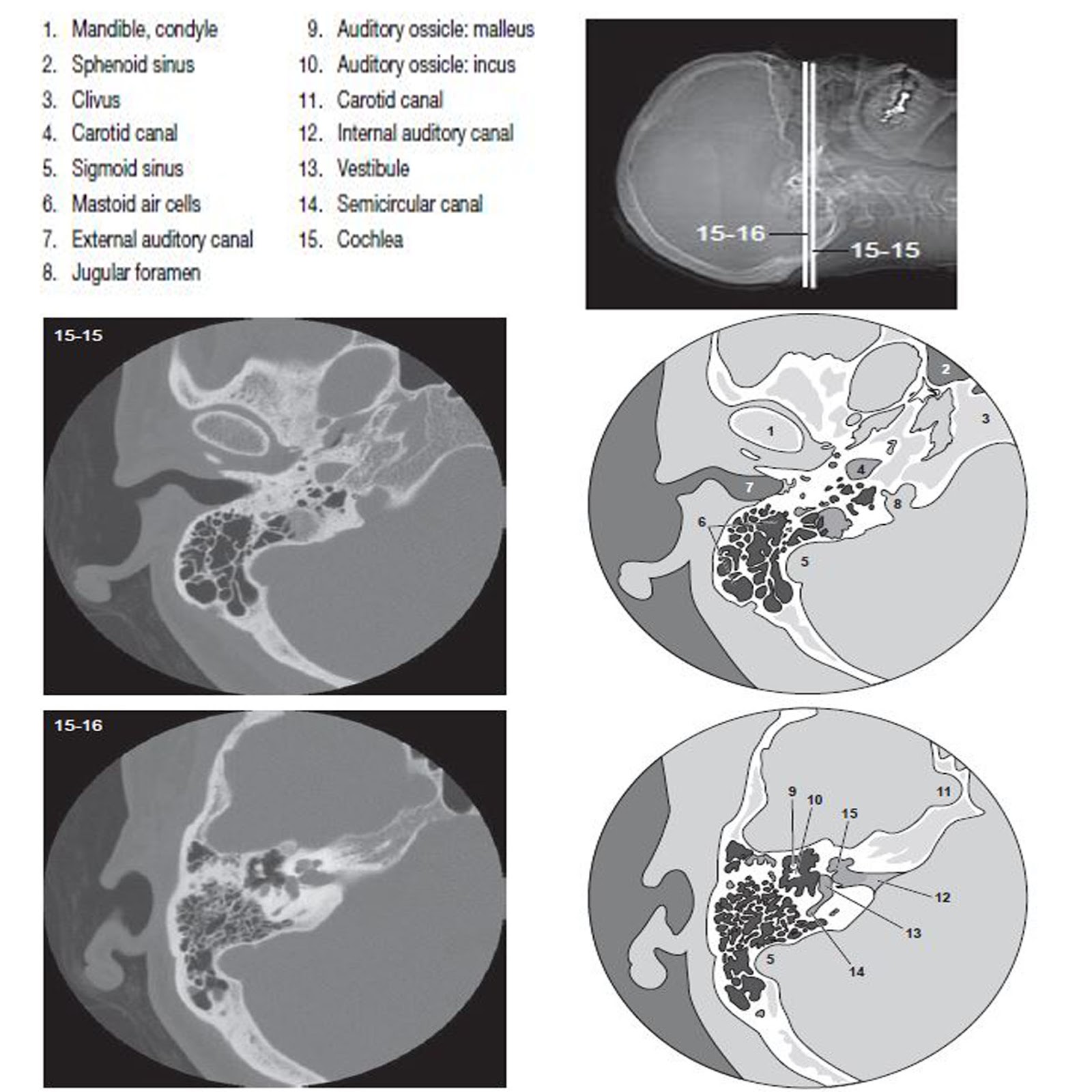
The temporal bone, often described as a symphony of ossification and anatomy, spans an area roughly 4 to 6 centimeters in height and width, with its architecture composed of several interconnected parts. These include the squamous, tympanic, mastoid, and petrous portions, each with distinctive features and clinical relevance. On high-resolution CT scans, the edges of these regions reveal a nuanced terrain of ridges, foramina, and air cells, all crucial landmarks for surgical navigation and diagnosis.
At the core of the temporal bone lies the petrous portion—a densely mineralized pyramid-shaped segment that encases the cochlea and vestibular apparatus. Its dense, compact structure appears as a hyperattenuating zone on CT, providing a stark contrast against the surrounding mastoid air cells and cavernous sinus. The lateral and anterior borders of the petrous part contribute to the formation of the middle cranial fossa and house critical neurovascular structures such as the internal carotid artery canal and the facial nerve canal. The squamous portion, forming the lateral wall of the skull, features the zygomatic process and the external auditory meatus—a conduit for auditory transmission. Meanwhile, the mastoid process, riddled with a honeycomb of air cells, plays a pivotal role in middle ear ventilation and infection pathways.
Evolutionary Context and Structural Significance
The evolutionary trajectory of the temporal bone underscores its significance in primate and human development. Its complex morphology reflects adaptations for auditory acuity, balance, and neurovascular protection. Over millions of years, the development of the petrous portion, with its dense bone, has served to safeguard vital inner ear structures from physical trauma while optimizing sound conduction and equilibrium functions. Current CT imaging not only reveals these functional adaptations but also exposes congenital variations and pathologic alterations that may challenge clinicians.
| Relevant Category | Substantive Data |
|---|---|
| Average volume of petrous portion | 65–70 mm³ in adults, providing sufficient space for inner ear structures—studies indicate minimal variation across populations |

CT Imaging Techniques: Shedding Light on the Hidden Structures

High-resolution CT (HRCT) remains the modality of choice for detailed visualization of the temporal bone’s anatomy. Utilizing thin slices—often 0.5 to 1 mm—coupled with multiplanar reconstructions, radiologists can generate detailed coronal, sagittal, and axial images. This approach unveils the subtle topographies of ossicular chains, tympanic cavity, facial nerve course, and inner ear labyrinths.
The advent of multi-detector CT (MDCT) technology has revolutionized temporal bone imaging by providing faster acquisition times and improved spatial resolution. Volume rendering and 3D reconstructions further assist surgeons in preoperative planning, especially for complex procedures like cochlear implantation or tumor resections. The imaging parameters, notably voltage (kVp), current (mA), and matrix size, are carefully calibrated to maximize bone contrast while minimizing radiation dose.
In pathology, CT excels at identifying ossicular discontinuities, erosions from cholesteatoma, labyrinthine fistulas, or vascular anomalies. Moreover, its capacity to detect subtle demineralization or sclerosis provides insights into osteitis and other inflammatory conditions affecting the periodontium of the temporal bone.
Advancing Visualization: From 2D Slices to 3D Reconstructions
The leap from traditional 2D axial slices to comprehensive 3D modeling allows for immersive visualization of complex anatomical relationships. Engineers and radiologists collaborate to craft virtual models that emulate real anatomy with astonishing fidelity. These models serve as invaluable tools for surgical rehearsal, patient education, and even augmented reality-guided interventions, marking an era where the unseen becomes vividly tangible.
| Relevant Category | Substantive Data |
|---|---|
| Imaging resolution | 0.5 mm slice thickness with 1024×1024 matrix in high-end HRCT scanners—enabling detailed visualization |
Pathological Considerations: What the Temporal Bone Reveals
The realm of temporal bone pathology is as rich and varied as its anatomy. From congenital anomalies to acquired diseases, CT provides a window into processes that can devastate hearing and balance if left unrecognized. Common conditions include cholesteatoma, osteitis, ossicular chain disruptions, and tumors such as acoustic neuromas or glomus tumors.
Cholesteatomas, characterized by keratinizing squamous epithelium proliferation, often manifest as soft-tissue densities eroding ossicles and the surrounding bone. HRCT displays their characteristic non-contrast soft-tissue masses with adjacent bony erosions—determinants crucial for surgical planning. Similarly, osteitis or sclerosis presents as increased bone density, while osteolytic lesions suggest infectious or neoplastic processes.
Trauma-related fractures may be linear or comminuted, with displacements affecting ossicular continuity or inner ear structures. Recognizing these breaks early through CT can dramatically influence treatment options, ranging from conservative management to extensive surgical repair.
Neoplasms and Their Imaging Signatures
Neoplastic processes within the temporal bone often pose diagnostic dilemmas owing to their proximity to critical neural pathways. Vestibular schwannomas or acoustic neuromas, for instance, present as characteristic intracranial masses that extend into the internal auditory canal, which CT can occasionally identify through bone remodeling and expansion, though MRI offers superior soft-tissue contrast. Conversely, glomus tympanicum and jugulare tumors primarily involve the middle ear and mastoid air cells, with CT revealing characteristic erosion patterns in ossicular chains and surrounding bones.
| Relevant Category | Substantive Data |
|---|---|
| Ossicular erosion | Present in approximately 75% of cholesteatoma cases—detected reliably via HRCT |
| Tumor bone erosion | Hyperdense or mixed-density areas with patchy or aggressive osteolytic changes—crucial diagnostic clues |
Future Directions: Enhancing Resolution and Surgical Outcomes
Emerging innovations in imaging technology continue to refine our understanding of the temporal bone. Ultra-high-resolution CT scanners, with slice thickness less than 0.3 mm, are now capable of revealing minute bone microstructures. Furthermore, integration with artificial intelligence (AI) algorithms enhances pattern recognition, predictive diagnostics, and personalized surgical planning.
Intraoperative navigation systems, built upon preoperative CT scans, are increasingly sophisticated, offering real-time guidance with sub-millimeter accuracy. The potential for augmented reality overlays directly onto the surgical field promises a future where visualizations are seamlessly integrated into operative workflows, reducing complications and improving outcomes.
Complementing imaging advances, bioinformatics and molecular genetics open new frontiers—understanding genetic predispositions to cholesteatoma growth or earbone dysplasia, enabling earlier diagnosis and targeted therapies.
Key Points
- Comprehensive knowledge of the temporal bone's anatomy enhances diagnostic and surgical precision.
- High-resolution CT facilitates detailed visualization, critical for pathology assessment and surgical planning.
- Technological innovations like 3D modeling and AI continue to augment understanding and clinical outcomes.
- Recognizing patterns of pathology on CT guides interventions, preserves function, and reduces complication rates.
- Future integration of intraoperative and bioinformatics tools holds promise for a completely new era in neuro-otological care.
What are the main components of the temporal bone visible on CT?
+The main components include the squamous, tympanic, mastoid, and petrous portions. These structures encompass critical features like the external auditory canal, middle ear cavity, mastoid air cells, and the dense petrous part housing the cochlea and vestibular apparatus.
How does CT imaging assist in diagnosing cholesteatoma?
+CT reveals soft-tissue masses with characteristic bony erosions, notably of ossicular chains and the long process of incus. The extent of erosion and adjacent bone destruction guide surgical management and prognosis.
What technological advancements are shaping future temporal bone imaging?
+Ultra-high-resolution CT, AI-powered pattern recognition, 3D virtual reconstruction, and augmented reality integration are rapidly enhancing the detail, accuracy, and intraoperative guidance capabilities of temporal bone imaging.