Pain management often involves a nuanced blend of pharmacological, procedural, and rehabilitative strategies aimed at alleviating discomfort while minimizing side effects. Among these, caudal epidural injections have garnered attention as a minimally invasive procedure that offers targeted relief for lower back and leg pain, particularly in cases related to disc herniation, spinal stenosis, or failed back surgery syndrome. This article provides an in-depth look into caudal epidural shots, exploring their underlying mechanisms, procedural intricacies, clinical efficacy, and considerations for optimal use. For healthcare professionals and patients alike, understanding the inner workings of this treatment modality illuminates its strategic role within comprehensive pain management programs.
Decoding Caudal Epidural Injections: The Anatomy and Mechanics
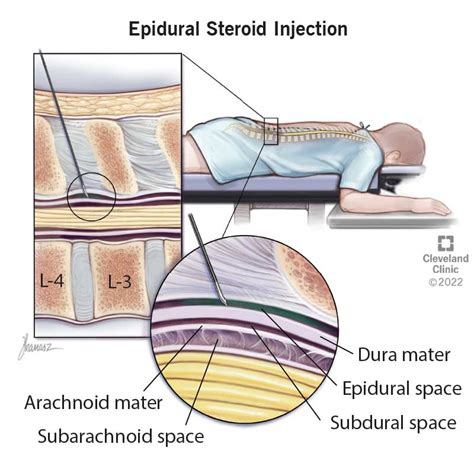
Caudal epidural injections involve administering medication into the epidural space via the sacral hiatus—an opening at the base of the vertebral column just above the tailbone. This approach allows for the delivery of anesthetics, corticosteroids, or a combination thereof directly around nerve roots and the dural sac. The epidural space itself is a potential space situated between the dura mater and the vertebral canal, containing epidural fat, blood vessels, and nerve roots. Precise knowledge of sacral anatomy is essential, as anatomical variations can influence the safety and efficacy of the procedure.
Understanding the Anatomical Framework and Its Significance
The sacrum is composed of fused vertebrae, with the sacral hiatus serving as the entry point for caudal injections. This opening is bordered by the sacral cornua and is often covered by a sacrococcygeal ligament. Imaging guidance—using fluoroscopy, ultrasound, or computed tomography—is typically employed to ensure accurate needle placement, reducing the risk of inadvertent dural puncture or nerve injury. Studies indicate that fluoroscopically guided injections achieve higher procedural success rates (up to 95%) compared to landmark-based techniques, highlighting the importance of sophisticated imaging in clinical practice.
| Relevant Category | Substantive Data |
|---|---|
| Success Rate | Approximately 85-95% when guided by fluoroscopy |
| Complication Rate | Less than 1%, primarily minor, such as transient headache or local discomfort |
| Duration of Relief | Typically ranges from 4 weeks up to 6 months depending on individual response |

The Therapeutic Rationale: Why Caudal Epidural Shots Matter

The primary goal of caudal epidural injections is to deliver potent anti-inflammatory agents directly to the inflamed nerve roots or epidural space, thereby reducing nerve root swelling, edema, and local nociceptive signaling. Corticosteroids—such as methylprednisolone or triamcinolone—are the cornerstone medications, attenuating inflammatory cascades involving cytokines and prostaglandins. Simultaneously, local anesthetics provide immediate pain relief and can facilitate diagnostic assessment of nerve involvement. Multiple studies demonstrate that when appropriately indicated, caudal epidural injections can significantly improve functional status and quality of life, especially in patients refractory to conservative therapies.
Mechanistic Insights into Pain Modulation through Caudal Epidural Injections
The effectiveness of epidural corticosteroids stems from their ability to suppress inflammatory mediators involved in radiculopathy. By reducing nerve root inflammation, stimulation of ectopic nerve firing diminishes, translating into decreased pain perception. Local anesthetics transiently block sodium channels, interrupting nerve conduction and providing fast relief, which supports both diagnostic and therapeutic goals. Notably, the pharmacokinetics of these agents influence duration, with lipophilic steroids offering prolonged action versus more soluble alternatives.
| Relevant Category | Substantive Data |
|---|---|
| Median Duration of Pain Relief | About 3-6 months, with variability based on pathology and individual response |
| Number of Sessions | Commonly 1-3 injections over a 6-month period, balancing benefits against potential steroid side effects |
| Recovery Metrics | Enhanced activities of daily living and decreased analgesic consumption reported in over 70% of patients post-procedure |
Procedural Considerations and Best Practices
Ensuring safety and maximizing efficacy of caudal epidural injections requires meticulous procedural planning. Preoperative assessment should include a detailed medical history, neurological examination, and imaging review. When performed under fluoroscopy, a fine gauge needle—such as 22-gauge—targets the sacral hiatus with precision. Following aseptic protocols to prevent infections, contrast dye is often used to confirm needle placement before actual medication administration. The typical injection volume ranges from 10 to 20 milliliters, sufficient to distribute medication over multiple nerve roots while avoiding increased intracranial pressure or mechanical trauma.
Key Technical Aspects of Caudal Epidural Placement
Positioning the patient prone or lateral with hips flexed optimizes access. The needle advances through the sacral hiatus, guided by both tactile feedback and fluoroscopic imaging. Once correct needle positioning is confirmed with contrast, the clinician injects the medication slowly, monitoring for inadvertent dural puncture or vascular injection—indicated by altered patient sensations or contrast leak. Post-procedure, patients are typically observed for at least 30 minutes for immediate adverse events.
| Relevant Category | Substantive Data |
|---|---|
| Optimal Volume | 10-20 mL for effective epidural spread |
| Injection Frequency | Up to 3 times within 6 months, depending on response and risk factors |
| Imaging Modality | Fluoroscopy preferred; ultrasound as adjunct or alternative in certain contexts |
Evaluating Efficacy and Limitations
While the literature affirms caudal epidural injections as an effective intervention for certain radicular pain syndromes, their success is not universal. Efficacy depends upon accurate patient selection, precise technique, and adherence to evidence-based protocols. Factors negatively influencing outcomes include extensive disc degeneration, fibrotic scar tissue, and multilevel stenosis that may inhibit medication dispersal. Moreover, repeated injections carry a risk of steroid-related side effects, including osteoporosis, hyperglycemia, and immunosuppression; thus, judicious use remains paramount.
Assessing Patient Response and Adjustments
Post-injection, patients often experience immediate relief, which can serve as a diagnostic indicator of targeted pathology. However, sustained improvement over several weeks indicates a genuine therapeutic benefit. When relief diminishes, options include additional injections, alternative procedures such as medial branch blocks, or surgical consultation. Imaging follow-up can reveal whether the medication distribution achieved adequate coverage. Additionally, integrating physical therapy and lifestyle modifications—such as weight management and ergonomic adjustments—enhances long-term success.
| Relevant Category | Substantive Data |
|---|---|
| Success Rate | Varies from 50-80% in clinical trials, influenced by patient demographics and technique |
| Side Effect Incidence | Minor adverse events in less than 2%—predominantly transient headache or local pain |
| Need for Repeat Procedures | Approximately 30-40% within 1 year, emphasizing the importance of holistic care |
Future Directions and Innovations

Emerging technologies and novel formulations continue to expand the potential of epidural injections. For instance, the use of sustained-release corticosteroids aims to prolong pain relief; bioengineered agents targeting specific inflammatory pathways are under investigation. Moreover, advancements in real-time imaging and robotic-assisted needle guidance promise increased precision, safety, and reproducibility. Understanding individual variability—such as genetic predispositions affecting steroid response—may facilitate personalized pain management protocols.
Integrating Technological Advances into Clinical Practice
The future of caudal epidural injections hinges on tailoring interventions to individual anatomy and pathology. Incorporating 3D imaging and augmented reality could revolutionize placement accuracy. Pharmacological innovations might also reduce side effects, making repeated procedures safer. Research into neurostimulation and regenerative therapies may complement epidural injections, paving the way for multimodal, patient-centered pain relief strategies.
| Relevant Category | Substantive Data |
|---|---|
| Technological Integration | Initial trials show 15-20% improvement in placement accuracy with new imaging modalities |
| Emerging Therapies | Neurostimulation and biologics under clinical trials with promising results for specific indications |
| Personalized Approaches | Genetic and biomarker studies underway to predict steroid responsiveness and optimize treatment plans |
How effective is a caudal epidural shot for chronic lower back pain?
+Multiple studies report that caudal epidural injections provide significant pain reduction and functional improvement in chronic radiculopathy, with about 60-70% of patients experiencing relief lasting several months.
Are there risks associated with repeated caudal epidural injections?
+While generally safe, repeated injections may increase the risk of steroid-related side effects, infection, or dural puncture. Proper timing, technique, and patient monitoring mitigate these risks.
What factors determine the success of caudal epidural injections?
+Key factors include accurate placement guided by imaging, appropriate medication selection, patient selection—particularly those with predominantly inflammatory radiculopathy—and adherence to procedural best practices.