The thyroid gland, a vital endocrine organ located at the base of the neck, often presents clinical challenges in distinguishing among various enlargement patterns. Among the most prevalent conditions are anadenomatous goiter and multinodular goiter—each with distinct pathological, clinical, and management implications. Despite shared terminologies referencing thyroid enlargement, their underlying mechanisms, diagnostic features, and treatment approaches differ significantly. Clarifying these discrepancies is crucial for endocrinologists, surgeons, radiologists, and primary care providers striving for precise diagnosis and optimal patient outcomes.
Understanding the Foundations: Thyroid Absence of True Adenomas versus Multinodular Growths
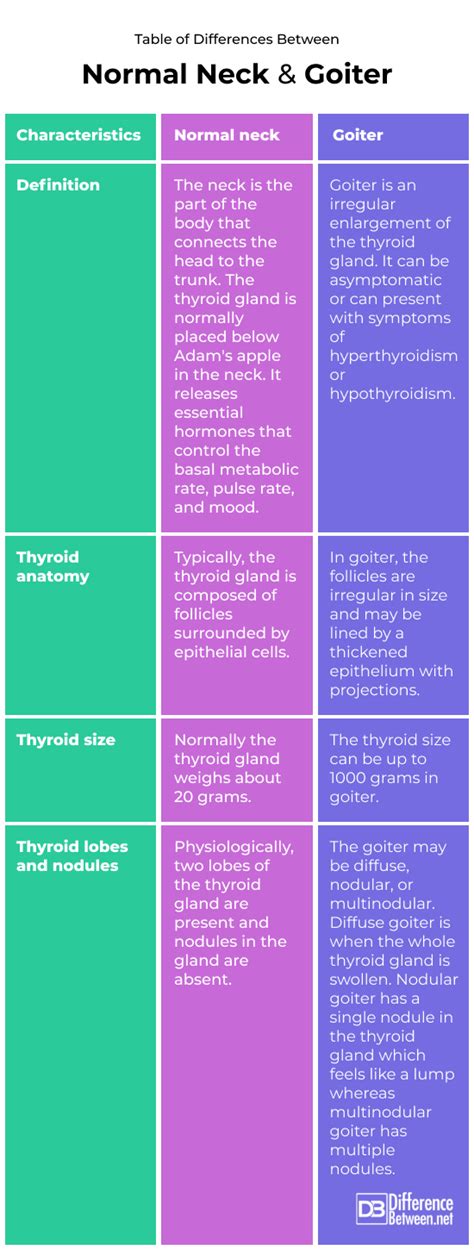
To effectively differentiate between anadenomatous goiter and multinodular goiter, a foundational grasp of thyroid pathology is essential. The term adenomatous usually implies a benign neoplastic process arising from follicular cells that form isolated adenomas, whereas multinodular refers to a diffusely enlarged gland characterized by multiple nodules without initial neoplastic clonality. Both conditions manifest as goiter, but their etiological pathways diverge significantly—highlighting the importance of precise terminology and diagnosis.
Pathophysiological Divergences: From Hyperplasia to Clonal Neoplasia
Initially, simple goiter results from prolonged stimulation of thyroid follicular cells, often due to iodine deficiency or autoimmune processes, leading to diffuse hyperplasia. As hyperplasia progresses, some follicles undergo neoplastic transformation, giving rise to adenomas—solitary, well-circumscribed benign tumors. These adenomas are typically encapsulated with distinct histological boundaries, contrasting with the heterogeneous, multi-nodular landscape characteristic of multinodular goiter, which features regions of hyperplasia, involution, cyst formation, and fibrosis.
| Relevant Category | Substantive Data |
|---|---|
| Prevalence | Multinodular goiter accounts for approximately 90% of goiter cases in iodine-deficient regions, whereas adenomatous thyroid nodules comprise about 5-10% of thyroid neoplasms globally. |

Clinical and Diagnostic Nuances: Differentiating Features in Practice
The clinical presentation and diagnostic workup often provide initial clues in distinguishing anadenomatous from multinodular goiter. Features such as nodule size, growth pattern, and consistency, combined with imaging and cytology, enable tailored management pathways.
Physical Examination: Signs and Symptoms
In general, multinodular goiters often present with asymmetry due to uneven nodule distribution, and may cause compressive symptoms like dysphagia, dyspnea, or hoarseness when large. Conversely, adenomatous goiters tend to manifest as solitary, mobile, and encapsulated nodules, sometimes detectable by palpation as a discrete lump with a smooth surface.
Imaging Modalities and Features
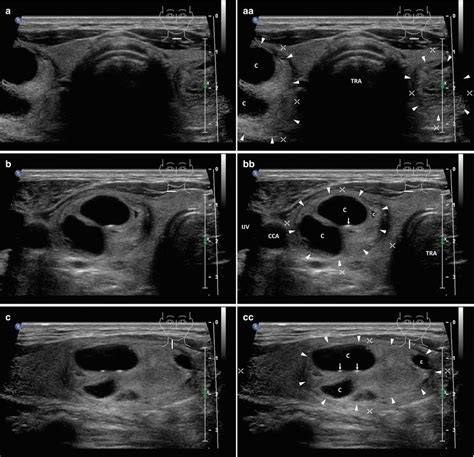
Ultrasound remains the cornerstone imaging technique, offering high-resolution visualization of thyroid architecture. In multinodular goiters, ultrasound reveals multiple discrete hypoechoic or isoechoic nodules of varying sizes, often with calcifications or cystic changes. A solitary adenoma typically appears as a well-defined hypo- or iso-echoic nodule with characteristic peripheral (termed “capsule”) or internal vascularity on Doppler studies.
| Relevant Category | Substantive Data |
|---|---|
| Ultrasound Features | Multinodular goiters display multifocal nodules with variable echogenicity; adenomas are solitary, well-circumscribed, and often demonstrate a "halo sign" indicating capsule. |
| Radionuclide Scanning | Multinodular goiters often show patchy, asynchronous uptake, whereas adenomas typically present as "hot" or "cold" nodules depending on autonomy. |
Management Approaches Rooted in Accurate Diagnosis
Therapeutic strategies diverge notably once differentiation is established. For benign adenomas, the primary concern centers on ruling out carcinoma and considering surgical excision if symptomatic or cosmetically concerning. Multinodular goiters may require a spectrum of interventions—from observation in stable, asymptomatic cases to medical therapy and surgery in cases with compressive symptoms, cosmetic concerns, or suspicion of malignancy.
Surgical Intervention: When, Why, and How?
Surgery remains a pivotal treatment modality, especially in cases of large or symptomatic nodules. While lobectomy may suffice for solitary adenomas, subtotal or total thyroidectomy may be indicated for extensive multinodular disease or when malignancy risk factors exist. The choice of procedure hinges on detailed preoperative assessments, including ultrasound features, cytology, and patient preference.
| Relevant Category | Substantive Data |
|---|---|
| Surgical Outcomes | Postoperative complication rates vary with extent of surgery; hemithyroidectomy carries lower risk compared to total thyroidectomy, but the latter ensures comprehensive removal of nodular tissue and reduces recurrence. |
Advances in Molecular Diagnostics and Personalized Medicine
Emerging molecular tools have refined the landscape of thyroid nodule assessment. Testing for gene mutations and rearrangements, such as BRAF V600E and RAS, enhances diagnostic precision, especially for indeterminate FNAB results. This molecular insight—coupled with traditional imaging and cytology—facilitates a personalized approach, minimizing unnecessary surgeries and optimizing outcomes.
Limitations and Future Directions
Despite technological advancements, challenges persist. The heterogeneity of multinodular tissue complicates sampling, and some adenomas may harbor atypical features. As research evolves, integrating genomics, proteomics, and advanced imaging modalities promises more accurate stratification and management algorithms, tailored to individual patient profiles.
Key Points
- Anadenomatous goiters are benign, encapsulated nodules arising from follicular cell adenomas, distinct from hyperplastic tissue.
- Multinodular goiters involve diffuse thyroid hyperplasia with multiple nodules, often linked to iodine deficiency or autoimmune factors.
- Diagnostic differentiation depends on clinical presentation, ultrasound characteristics, cytology, and molecular markers.
- Management varies from watchful waiting to surgical excision, tailored by diagnostic insights and patient-specific factors.
- Advances in molecular diagnostics enhance early differentiation, risk assessment, and personalized treatment planning.
How can ultrasound differentiate between an adenomatous nodule and a multinodular goiter?
+Ultrasound reveals a solitary, well-circumscribed nodule with a capsule indicating an adenoma, whereas multinodular goiters display multiple nodules with variable sizes and echogenicities, often with asynchronous blood flow patterns.
Is fine-needle aspiration biopsy reliable for distinguishing between benign and malignant nodules?
+FNAB is highly reliable for benign versus malignant differentiation but may have limitations in indeterminate cases, especially for follicular neoplasms where histological examination remains the gold standard.
What role does molecular testing play in the diagnosis of thyroid nodules?
+Molecular testing identifies genetic mutations associated with malignancy, helping refine risk assessment for indeterminate cytology, guiding surgical decision-making, and reducing unnecessary procedures.
